Getting the Drop on Better Health
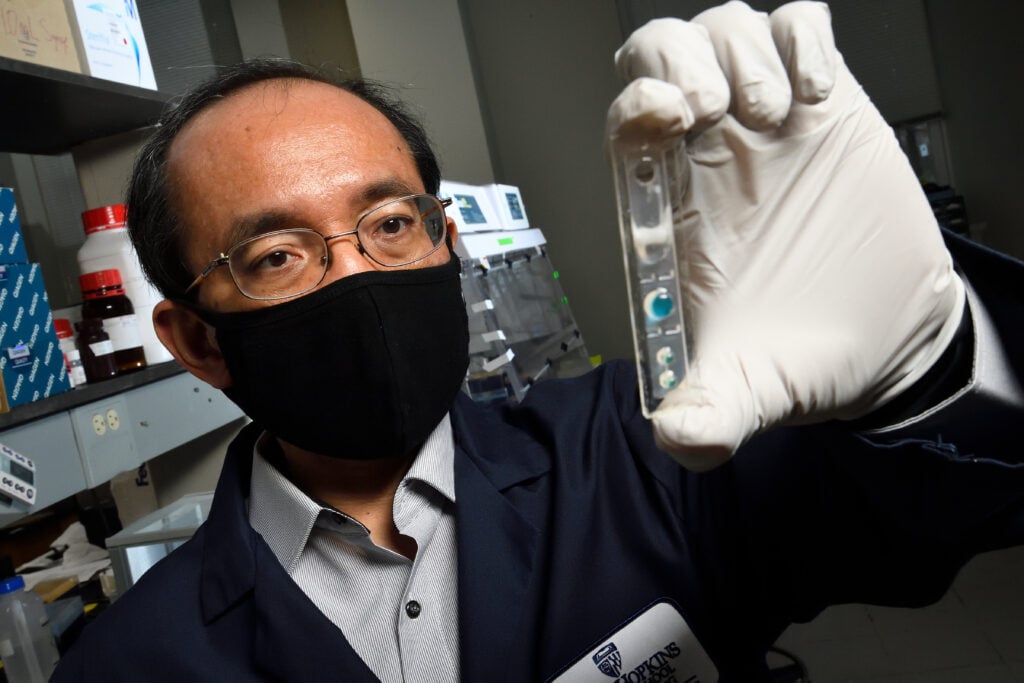
Professor of mechanical engineering Tza-Huei (Jeff) Wang spends his days working with tiny droplets of fluid. Some of his lab’s devices analyze droplets that are one-millionth of a liter. Others use a far smaller scale: one-trillionth of a liter.
Why would anyone want to isolate such minute volumes of fluid? Because microfluidics, as Wang’s field is known, allows rapid, precise analysis of many kinds of biological processes.
Over the last decade, Wang’s lab has developed devices that might someday make it far easier for clinicians to identify infectious pathogens and to diagnose early-stage cancers. And because some of these devices have the potential to be cheap and portable, they might transform health care in low-resource countries that have few traditional hospital laboratories.
“With microfluidics,” Wang says, “you can control the microenvironments you want to look at. You have precise temporal and spatial control. You have resolution even down to the single-cell level. It’s a very elegant approach.”
To translate his lab’s technologies into real-world clinical progress, Wang has built collaborations with a broad team of physicians and epidemiologists at Johns Hopkins and elsewhere.
One of Wang’s highest-profile recent projects involves a portable device that can rapidly confirm an infection with gonorrhea—and, remarkably, can identify within 15 minutes whether the gonorrhea will respond to traditional antibiotics. In a typical hospital lab, that process takes two to four days. But with Wang’s device, a patient can receive a diagnosis and start treatment, all within a 45-minute clinical visit.
“It’s a huge benefit to start treating the patient during that initial visit,” says Charlotte Gaydos, a professor of infectious diseases at the Johns Hopkins University School of Medicine, who has collaborated with Wang for more than seven years. “Usually, you’re waiting several days for results to come back, and during that time, there’s a risk of further transmission of infection.”
Wang, Gaydos, and their colleagues have tested their device in the Emergency Department at the Johns Hopkins Hospital and at several clinics in Baltimore. They have also piloted the system in rural areas of Uganda, where antibiotic-resistant gonorrhea is becoming prevalent.
At each site, Wang has worked to make sure that the device actually fits into the local clinical workflow. “Ten years ago,” he says, “some people were very, very frustrated with microfluidics because we’d invented all of these very elegant, very powerful microchips, but they couldn’t be used easily in clinical settings. People didn’t see a lot of actual real-world products.”
To avoid that pitfall, Wang teaches his graduate students and postdocs to have long, deep conversations with their physician collaborators. “Don’t just read their papers,” he says. “Go and visit their clinics and see how the work actually happens.”
Using that collaborative approach, Wang’s lab has developed an array of devices for detecting cancer and analyzing pathogens. With Stephen Meltzer, a professor of oncology at Johns Hopkins, Wang has developed a new technique for detecting precancerous changes in the esophagus. With Karen Carroll, a professor of pathology, he has developed a microfluidic platform that can accurately identify any of dozens of pathogens in a tiny specimen of urine. Like the gonorrhea device, this platform can deliver extremely fast reports about the pathogens’ sensitivity to antibiotics.
Pushing the Limits
Wang was raised in Taiwan, and he earned his bachelor’s and master’s degrees there. He worked for two years in the mid-1990s at a major Taiwanese semiconductor firm, where he found himself becoming a bit bored. “As an entry-level engineer,” he says, “the scope of your work was quite limited.”
He started to hear about the emerging field of microelectromechanical systems—the science of developing small sensors combined with tiny mechanical elements. (Think of the proprioceptive sensors that tell your cellphone which way is up.) In 1998, he successfully applied to the doctoral program at UCLA, which was a pioneering center of MEMS research.
“The UCLA program was very exciting,” he says. “At that time, not many people were interested in applying MEMS techniques to biomedical problems. But there were a handful of us there who wanted to make it happen.”
An early project at UCLA involved a Defense Department grant for developing small devices that could detect anthrax or other biowarfare agents. “My challenge was to try to push these devices to the fundamental limit,” Wang says. “We wanted to see whether you could transduce DNA-binding events to an optical signal detectible at the single-molecule level.” It was this project, Wang says, that provided the proof of concept for all of his subsequent work in microfluidics.
Wang arrived at Johns Hopkins as a junior faculty member in 2002. He was hired directly from UCLA, without having completed a postdoctoral fellowship. “I was quite stressed at the beginning,” he says, “because I didn’t have much teaching experience. I didn’t have experience writing grants. I knew that the tenure clock would start ticking as soon as I set foot on campus. But I had great support from senior faculty, and it all worked out well.”
Gaydos, Wang’s collaborator on the gonorrhea device, says she appreciates his flexibility and his willingness to reach across disciplines. “When I first started to work on point-of-care devices for sexually transmitted infections,” she says, “Jeff approached me and said he had technology for cancer diagnosis—detecting single-nucleotide polymorphisms—that we might be able to apply to identifying antibiotic susceptibility. He dove right into the problem.”
Wang says that his visits to the Ugandan clinical sites in 2019 were among the most valuable experiences of his time at Johns Hopkins. “While I was there,” he says, “I heard about a problem I’d never even thought about. Clinics in Uganda sometimes get shipments of counterfeit antibiotics, and they can’t tell what’s real. So that might be my next project: a portable device for the rapid authentication of medicines.”
The new generation of doctoral students in engineering, Wang says, tends to be highly committed to that kind of practical, translational work. “I don’t mean that basic science isn’t exciting,” he says. “It’s very exciting. But the students I see today also want to make an impact in the real world.”
Wang and his colleagues are preparing to have a few of their pathogen-detecting devices cleared for use by the FDA. Before long, his lab’s work with tiny droplets could have an enormous impact.
Story from the summer 2021 issue of JHU Engineering Magazine. Story by David Glenn. Photo by Will Kirk.